Dan Morgan
@dr_dmorgan
Followers
4K
Following
10K
Media
240
Statuses
3K
ID doctor and epidemiologist creating pragmatic solutions for hospital isolation, better diagnosis and AI for patient safety metrics.
Baltimore, MD
Joined November 2014
How good are doctors at diagnosis? This is the most relevant paper I have written. Not perfect but addresses a huge issue I think could change medicine if acknowledged …it has changed how I think about diagnosis https://t.co/4ZtoD3F4rF
@JAMAInternalMed
@drjohnm 1/n
jamanetwork.com
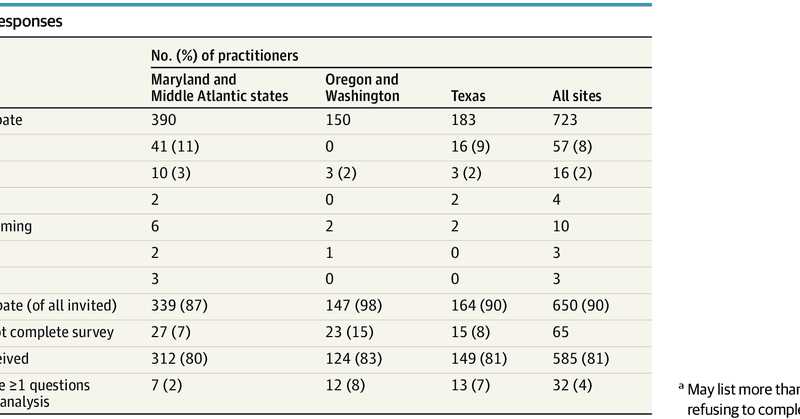
This survey study of physicians, nurse practitioners, and physician assistants explores practitioner understanding of diagnostic reasoning.
40
209
669
Ep 3: Diagnostic stewardship with @dr_dmorgan
https://t.co/2Xriz5mMYX
https://t.co/Z7K26M11iy
https://t.co/G8sQGWImwC
1
1
4
At the @SHEA_Epi conference, Valeria Fabre talking about diagnostic stewardship! @ValerieVaughnMD
0
0
6
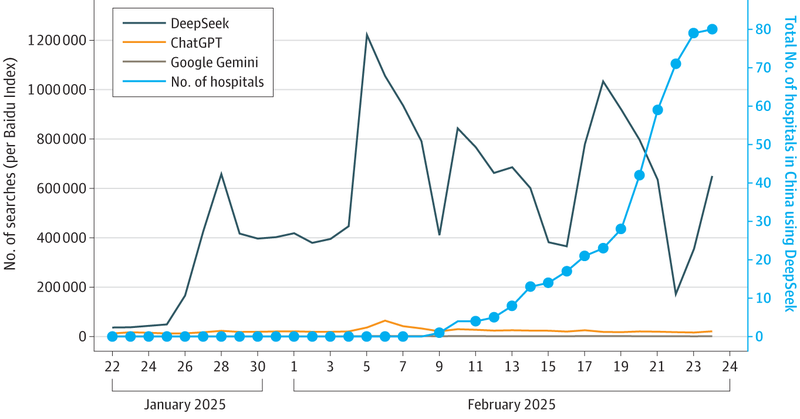
Wild to hear about DeepSeek being used in Chinese hospitals. Seems risky but a snapshot of where things are going..... Worth a read @AdamRodmanMD @PreetiNMalani
jamanetwork.com
This Perspective examines the rapid adoption of DeepSeek, a large language model, across Chinese hospitals and the regulatory and governance concerns surrounding the use of artificial intelligence–...
0
0
4
Requirement to throw away most medical equipment after single use is largely driven by extra barrier by @FDA to prove safe to reuse. @DrMakaryFDA, would you reconsider this? @SHEA_Epi conference
0
0
7
Annual N95 fit-testing is still required based on 1 small study of 229 participants. In a study of 12,065 HCWs followed over 3 yrs, fit‑test failure was <0.5% (Martin et al). Annual fit‑testing still costs US healthcare ~$200–400 M/yr. Time to switch to every 3 years.
4
7
38
Great to hear about these SNAP trials, @DrEmilyMcD !
It’s happening now! The results of the SNAP PSSA and MSSA domains Recently, the number of patients recruited in SNAP surpassed all randomized patients in staph aureus trials combined! #ESCMIDGlobal2025
@syctong @DrToddLee
0
0
9
De-Baathification was.... not a successful policy... like... famously... it was the source of most of America's challenges in Iraq for the years that followed... seems like maybe it really is an apt metaphor for the current strategy...
JD Vance: “We need a De-Ba’athification program in the U.S....We should seize the administrative state for our own purposes. We should fire … every civil servant in the administrative state. Replace them with our people.”
4
19
108
Among the 12 most commonly diagnosed cancers in the US, we found striking variability in the incidence/mortality relationship – with correlation coefficients ranging essentially from 0 (breast and thyroid cancer) to 1 (lung cancer): https://t.co/cCyOcOe7Iy
1
4
16
Great work @JonBaghdadi
Across ~750k inpatients in 928 U.S. hospitals, starting with empiric narrow-spectrum antibiotics escalated to broad-spectrum antibiotics based on cultures was NOT associated with worse outcomes compared with empirically starting broad.
0
0
1
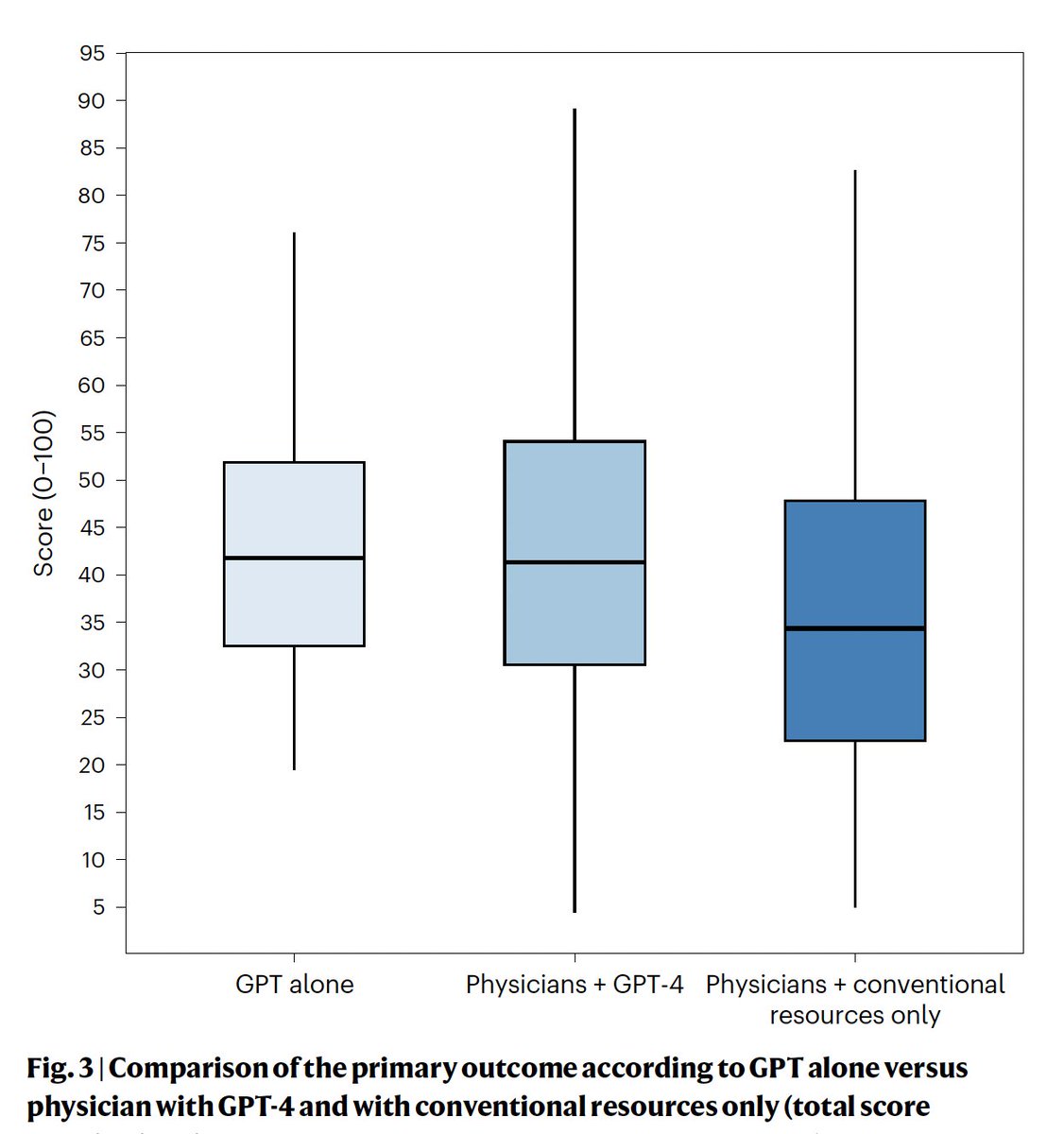
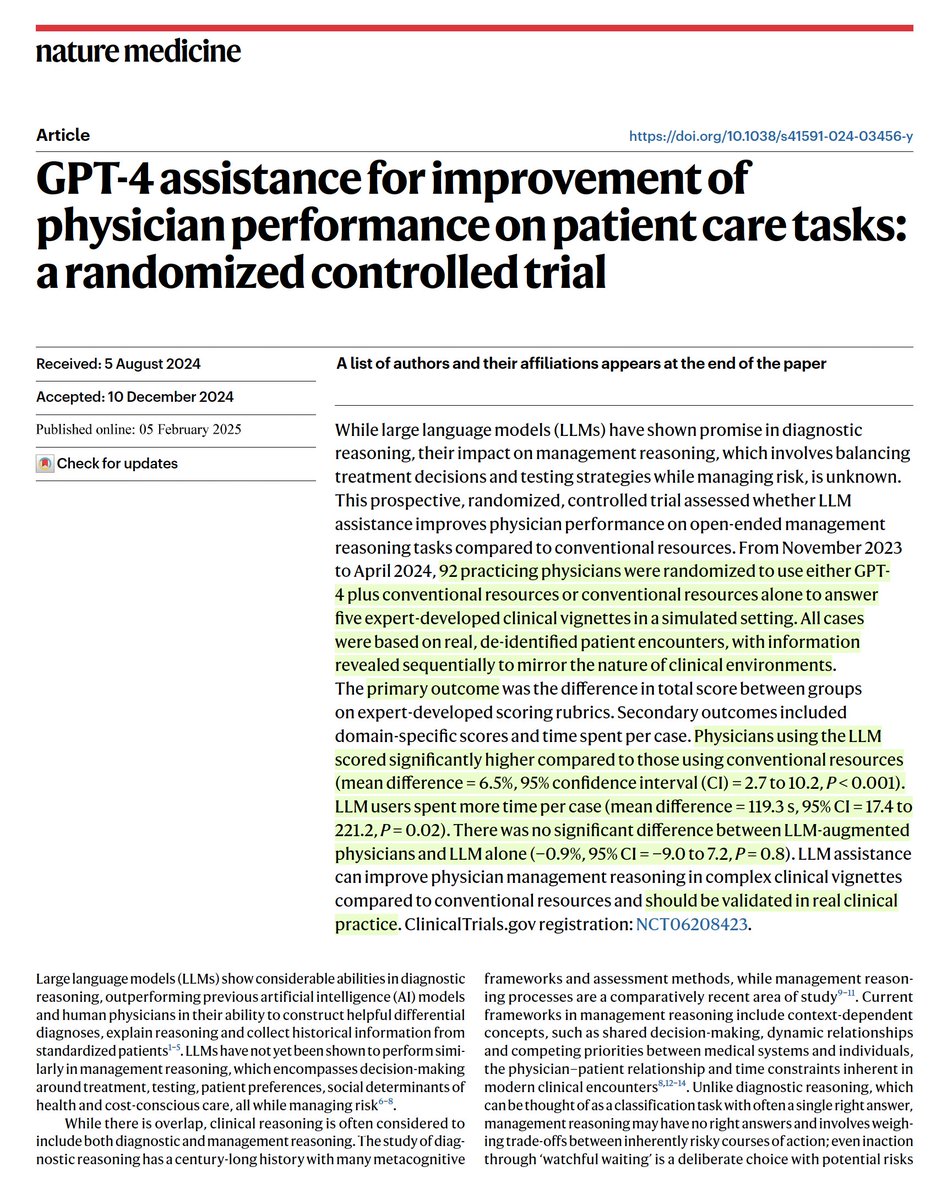
There is a lot of buzz about our new paper in Nature Medicine on the effects of LLMs (GPT-4) on physician management reasoning! I had TONS of fun working on this -- but what it MEANS requires some unpacking. A 🧵⬇️ https://t.co/yLZJw1U5IE
A randomized trial of GPT-4 vs 92 physicians with or without this #AI LLM for performance on patient care tasks. AI improved physician performance, on par with AI alone (based on 5 clinical vignettes) https://t.co/c7b82kQLi8
@NatureMedicine @AdamRodmanMD @jonc101x
8
94
284
Great to see talk about Mindlines, evoking the great BMJ paper about actual clinical practice.
Are clinicians’ beliefs & emotions key drivers of their antibiotic prescribing? 🆕💫 Sub study INHALE Guidelines vs mindlines: a qualitative investigation of how clinicians’ beliefs influence the application of rapid molecular diagnostics in intensive care https://t.co/RvuAwtrRlw
1
1
5
Articles like this wear me out. It comes so close to discussing real problems - then parrots back the same platitudes. Do we *really* need more doctors? Or do we need a system that incentivizes doctors to practice in the ways/places we need, instead of doing the very opposite?
Physician shortages in the United States are projected to worsen, especially in rural areas. Dr. @RWalensky and @NCMcCann argue that broad reforms, including changes in education and compensation, are needed. Read the full report: https://t.co/NUayk59LnW
45
58
554
Diagnostic stewardship, which extends to clinical medicine, and laboratory stewardship serve complementary roles & collaboration allows both programs to grow and improve patient care. Mini-Review by @ClaeysKcclaeys, KC Coffey & @dr_dmorgan:
0
2
5
The use of oseltamivir in the total absence of evidence of benefit meets the criteria of therapeutic fashion. Evidence-based practice has a long way to go.
The Limited Role for Antiviral Therapy in Influenza commentary on a SR/MA with @JonBaghdadi "When considering the evidence, we are left to wonder why reflexive treatment of influenza with oseltamivir has become so ingrained in clinical practice." https://t.co/mqL4O4JELn
0
13
18
Same group wrote: Same group examined hospitalized patients "in severe influenza, oseltamivir and peramivir might reduce duration of hospitalisation compared with standard care or placebo, although the certainty of evidence is low." https://t.co/Y3wxKa4lfK
thelancet.com
In hospitalised patients with severe influenza, oseltamivir and peramivir might reduce duration of hospitalisation compared with standard care or placebo, although the certainty of evidence is low....
0
1
5
I know some asked for the manuscript. Hopefully this screenshot is clear. We wrote a note on a SR/MA that included grandfather of EBM, @GuyattGH
https://t.co/AUNogHC64D
1
1
3
The Limited Role for Antiviral Therapy in Influenza commentary on a SR/MA with @JonBaghdadi "When considering the evidence, we are left to wonder why reflexive treatment of influenza with oseltamivir has become so ingrained in clinical practice." https://t.co/mqL4O4JELn
10
24
91
But we know how to test efficacy in medicine. Clinical trials are messy, more expensive than in silico studies, and require multidisciplinary expertise. But they're still the right thing to do. Only 5% of LLM in medicine studies even use real data ( https://t.co/gc2sl3VFYn)!!
pubmed.ncbi.nlm.nih.gov
Existing evaluations of LLMs mostly focus on accuracy of question answering for medical examinations, without consideration of real patient care data. Dimensions such as fairness, bias, and toxicity...
1
4
23