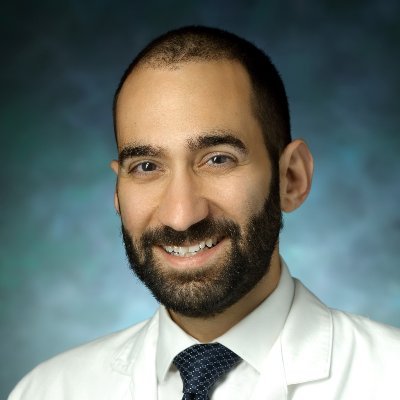
Phil Bilodeau, MD
@phil_bilodeau
Followers
2K
Following
6K
Media
117
Statuses
1K
Neuroimmunology 🧠 🔥 clinician scientist @MGHNeurology, @BWHNeurology. Grad of @harvardneuroMDs & @mcgillmed.
Boston, MA
Joined December 2011
Why has no one thought of opening a bar near a hospital and calling it PubMed
246
3K
22K
I am very grateful to @PCORI for funding our clinical trial on the comparative effectiveness of immunotherapies in NMOSD. Huge shout-out to our entire team: @TheSumairaFDN, Prof. Friedemann Paul, and Dr. Marcelo Matiello, without whom this would not have been possible.
0
2
21
I make a point of deleting the handedness out of every one-liner…Mostly useless piece of information which only bloats the notes
Controversial neurology opinion of the day: the weird obsession we have of presenting the patient’s handedness as super important (“this 57 right-handed male…” etc) is almost never of any real clinical value. (Don’t hate me cognitive people!)
1
0
6
Absolutely brilliant read from @tompollak about the dangers of attributing everything to inflammation. I would add that we, as a field, cannot even agree on what constitutes pathologic inflammation. https://t.co/c8Rby65E8D
academic.oup.com
Thomas Pollak explores the emergence of a new worldview which attempts to explain all manner of ills as the result of inflammation or immune dysfunction. H
3
3
19
If you treat MOGAD patients, check out our editorial on B-cell depletion in MOGAD! https://t.co/xo3RIMh9ay
1
8
28
Interesting study. Need to be careful though with potentially overinterpreting this and other retrospective observational studies purported to prove the effectiveness of early PLEX. My detailed rapid response to this article is here:
jnnp.bmj.com
Background Incomplete attack remission is the main cause of disability in myelin oligodendrocyte glycoprotein antibody-associated disease (MOGAD). Apheresis therapies such as plasma exchange and...
Apheresis therapies in MOGAD: a retrospective study of 117 therapeutic interventions in 571 attacks https://t.co/bUToBLxPsj
@NeuroVisionLab
1
6
14
0
0
1
Very important paper our lab led by Dr. Natalia Drosu. We identified DR15-restricted epitopes recognized by EBV-specific CD4 T cells. Findings support the use of antiviral therapies/antigen-specific deletion of EBV-targeting CD4 T cells in MS. https://t.co/FKCw8StzqO
1
15
42
🔍Editor’s Choice Paper 🛎️Welcome to this review "The Impact of Anti-Amyloid Immunotherapies on Stroke Care". ✍️by @phil_bilodeau et al. @MarielKozberg 🔗More details: https://t.co/wBye2vs5em
@MediPharma_MDPI @harvardmed
#mdpijcm #Stroke #neurotwitter
How will anti-amyloid immunotherapies and ARIA affect stroke care? @phil_bilodeau, John Dickson, and I review the latest data on ARIA in the context of acute stroke care and secondary stroke prevention here:
0
2
1
#RTwitter, any straightforward way of incorporating iptw weights into brms when doing a Bayesian analysis?
0
0
2
This! Always keep MOG on your differential for cortical encephalitis and remember it may not be on the autoimmune encephalopathy panel (for Mayo it is not).
1/ A 34 yo M presents with worsening confusion and seizures. He is febrile. He is intubated and transferred to the NeuroICU. A #continuumcase about a cause that’s probably low (not) on your DDx.
0
5
24
Great thread! Would also mention tocilizumab as an acute treatment for fulminant ADEM esp if intracranial hypertension.
neurology.org
ObjectivesMyelin oligodendrocyte glycoprotein antibody-associated disease (MOGAD) is an immune-mediated neuroinflammatory disorder leading to demyelination of the CNS. Interleukin (IL)-6 receptor...
A 19 year old is brought to the ED after 2 days of progressive confusion and drowsiness Last week he had a fever and runny nose. Got better. He soon becomes unresponsive and requires intubation This is his MRI performed the next day. What’s going on? What do you do?
0
1
4
Congratulations to @shamik_b, the inaugural incumbent of the Anne Finucane Distinguished Chair in Neurology. Dr. Bhattacharyya was celebrated during an event on May 20th.
6
4
49
Very grateful for the support of Banting Canada for my postdoctoral fellowship. I will studying the role of gamma delta T cells in MS. Also incredibly grateful to my mentors @mlevy18 @shamik_b for their support! Stay tuned! @BWHNeurology @harvardmed
Today, Ministers Holland and Champagne announced the recipients of the 2024 #VanierCanada and #BantingCanada awards. These talented doctoral students and postdoctoral researchers are the future leaders of innovation and research excellence in Canada. https://t.co/CzRWSHq1yj
2
2
23
In a recent study published in the Journal of Brain, Behavior, and Immunity, researchers from @MGHNeurology and colleagues investigated MS and synapse damage from inflammation. Read more: https://t.co/43nlyVmSYt
@mghneurosci
0
4
6
His portrait hangs in the hearts of his students. "Si monumentum requiris circumspice."
This evening we unveiled the portrait of the late Martin A. “Marty” Samuels, M.D. in the Wolf Conference Center. This portrait will hang in the Department of Neurology @BrighamWomens. Thank you to Warren and Lucia Prosperi for their hard work on this incredible piece!
0
4
18
Among 258 people with #MultipleSclerosis treated with monoclonal antibodies (natalizumab, ocrelizumab, ofatumumab, rituximab), 54.7% had wearing-off phenomenon, along with depression and poor treatment satisfaction. Online survey from @ClevelandClinic ▶️ https://t.co/wpMPaN4ZRg
2
12
33
With the advent of BTK inhibitors in MS, we’ll have to be even more careful and advise patients on the risks
BTK inhibitors increase the risk of Aspergillus infections. Our new paper shows that these drugs blunt antifungal activities by neutrophils. How does this happen, and can we recover function? (1/5)
0
1
5
Happy to share @Lauz_Caccia et al study of #MOGAD lesion changes during attacks: ➡️ 10% of attacks have an initial normal MRI (radiologic lag) ➡️ MRI more dynamic than in #MS or #NMOSD with T2-Lesions often appearing & sometimes resolving within attacks👇 https://t.co/8ju2xF2y46
1
26
87
We investigated whether HSV encephalitis is associated with having systemic autoimmune disease or exposure to immunosuppression. In the Medicaid dataset, there was a positive association on both counts! https://t.co/AuWltHiX5y
neurology.org
Background and ObjectivesAmong infectious etiologies of encephalitis, herpes simplex virus type 1 (HSV-1) is most common, accounting for ∼15%–40% of adult encephalitis diagnoses. We aim to investig...
1
4
35
So many “UTIs” that turned out to be HSV encephalitis. As @eemoin said, just because a test is negative doesn’t mean it wasn’t indicated
@theBSinBSN Have I seen patients die of encephalitis because someone with lesser diagnostic acumen called it "urosepsis" ? Yes. Too many times.
1
0
10