Elias Sotirchos
@ESotirchos
Followers
441
Following
169
Media
1
Statuses
88
Neurologist @HopkinsMedicine with interests in #MultipleSclerosis #NeuromyelitisOptica #MOGAD #Neuroimmunology
Baltimore, MD
Joined April 2018
Happy to share @albertaboseif et al multicenter study showing 4% of #MOGAD with meningitis ➡️ Frequent misdiagnosis as infection ➡️ Updates in criteria could incorporate this phenotype ➡️ Path had meningeal T & B cells, microglia & cortical myelin loss👇 https://t.co/7gn8z4HzhH
1
36
85
Delighted to share Kwon & @NanthayaTisa et al study with our Korean colleagues led by Dr Sung-Min Kim ➡️ We found paraneoplastic #MOGAD is rare & tumors lacked MOG immunostaining making the mechanism of this infrequent association uncertain 👇 https://t.co/N5iFQXVL20
0
16
47
Among 190 people with MOG antibody-associated disease #MOGAD, relapses were more frequent in the group with CSF-restricted oligoclonal bands, particularly within the first year of follow-up. Study from @CHUdeLyon @marignierro ▶️ https://t.co/XTq8tjluGb
1
13
33
In these situations, especially if live CBA is not available for follow-up testing in patients with high suspicion for MOGAD or AQP4+ NMOSD, clinical and imaging phenotypic characteristics need to be relied on more heavily to help guide appropriate management.
0
2
6
We must recognize though that fixed CBAs may be the only assays readily accessible, especially in resource-limited settings.
1
1
3
These results support that using exclusively fixed CBAs may miss many cases resulting in misdiagnosis and consequently suboptimal treatment, but also has significant implications for characterizing "double-seronegative" NMOSD.
1
1
5
Live CBA had markedly better sensitivity, especially for MOG-IgG testing, with very good specificity for both live and fixed CBA (notably specificity was 100% for AQP4-IgG by both assays).
1
1
3
Excited to share out study led by @_YanaSaid and in collaboration with the Mayo clinic group (including @EoinFlanagan14 @chenmayo ) reporting our real-world clinical experience with paired fixed and live CBA testing for MOG-IgG and AQP4-IgG. https://t.co/jJZVPUccNq
onlinelibrary.wiley.com
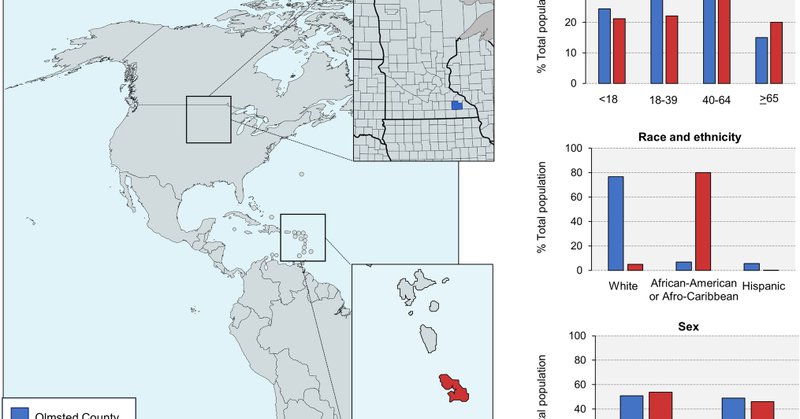
Objective To assess the real-world performance of a live (LCBA) versus a fixed (FCBA) cell-based assay for the detection of serum antibodies directed against myelin oligodendrocyte glycoprotein...
1
5
17
When do drugs really expire? Which ones take decades to degrade? Why does the US government use secret expiration dates for pharmaceutical stockpiles — but make pharmacies & hospitals discard perfectly potent meds? I went down a wild rabbit hole for us
163
1K
6K
If you don't know much about PBMs, you can learn more below: https://t.co/VE3vujvVk3
THREAD: There is a massive, totally legal bribery scheme driving up drug prices in America. And pharmacy benefit managers—shady middlemen you’ve probably never heard of—are right at the center.
2
43
170
A multi-center, randomized-controlled, open-label, rater-blinded, pragmatic trial “Treatment of Inflammatory Myelitis and Optic Neuritis with Early vs Rescue Plasma Exchange” that is planned to commence in the United States in 2025.
0
0
1
Regardless though, a randomized controlled clinical trial is needed to further inform the use and timing of PLEX for treatment of severe demyelinating attacks. This is why we are pursuing (together with co-PI @chenmayo), the TIMELY-PLEX trial:
1
0
0
Performing additional analyses, including a formal comparison of 1st-line PLEX recipients vs those who received only corticosteroids, accounting/matching for relevant variable such as demographics, attack severity etc can help provide further insight into these findings.
1
0
0
So unless we think that PLEX actually worsens clinical outcomes (which seems unlikely), it should be fairly clear that this is likely driven by selection bias.
1
0
0
Notably, in this study patients treated with only corticosteroids for their attacks had BETTER disability than those who received PLEX at the last follow-up, despite similar demographics and clinical characteristics.
1
0
0
This is a huge selection bias that is present in all retrospective studies of PLEX in NMOSD and MOGAD, since the analysis is restricted only to those who received PLEX.
1
0
0
PLEX is not done as a 2nd or 3rd-line therapy randomly, but because patients did not significantly improve or even worsened after 1st line therapy. Conversely, many of those who received PLEX as a first-line therapy may have improved with just corticosteroids.
1
0
0
Interesting study. Need to be careful though with potentially overinterpreting this and other retrospective observational studies purported to prove the effectiveness of early PLEX. My detailed rapid response to this article is here:
jnnp.bmj.com
Background Incomplete attack remission is the main cause of disability in myelin oligodendrocyte glycoprotein antibody-associated disease (MOGAD). Apheresis therapies such as plasma exchange and...
Apheresis therapies in MOGAD: a retrospective study of 117 therapeutic interventions in 571 attacks https://t.co/bUToBLxPsj
@NeuroVisionLab
1
6
14
I had a great time talking with @DrewCareyMD, and have to give a shout out to Sinan Akosman for spearheading the project and @Meditav063 for co-mentoring. Can’t wait for our upcoming PCORI funded clinical trial on early PLEX for severe ON and TM with co-PI @ESotirchos!
Always have a great time talking with @chenmayo from @mayoclinic about his exciting research into #OpticNeuritis, listen to our recent conversation on the use of plasma exchange (PLEX) as rescue therapy #NeuroOphth #eyetwitter #neurotwitter
0
5
20