Lin Chang
@LinChangMD
Followers
2K
Following
2K
Media
51
Statuses
991
Vice Chief, #UCLAGI | Director, GI Fellowship Program @UCLAHealth | IBS, Brain-Gut, DGBI | ❤️ Translating Science to Improve Patient Care | Tweets my own
Los Angeles
Joined July 2021
AGA's new quality indicators for #IBS set the standard for improving patient care! Learn about these standards, which were developed to enhance diagnosis, treatment, and outcomes of IBS. Don't miss this important read! 📖👇 #GIQuality
Are you providing high-quality #IBS care? Here are 9 quality indicators that AGA and @RomeFoundation recommend to improve and standardize care ➡️ https://t.co/Rt7mwxS4Up Thanks to the team: @JenniferKMaratt @LinChangMD @RabWatsonMD @KazaArchana @David_LeimanMD @KennethHung17
1
4
34
Excited to welcome this incredible group of future gastroenterologists to #UCLAGI! #Match2026 🐻 ⭐️Prahan Chetlur, MD ⭐️Angel Alejandro Campos Rodriguez, MD ⭐️Minh Do, MD ⭐️Stephanie Kim, MD ⭐️Krystal Lai, MD ⭐️Austin Peer, MD, MPH ⭐️Nicholas “Nico” Valle, MD ⭐️@KemingYangMDPhD
0
5
25
Biomarkers in Irritable Bowel Syndrome: Rational and Practical Use🔖Gastroenterology Clinics of North America 🔑Read more about promising noninvasive diagnostic and therapeutic biomarkers in #IBS 👥 @Michelle8Guan @LinChangMD 👉 https://t.co/64K0MrnyAG
0
13
23
Extraintestinal Symptoms in #IBS are Associated with Stress Reactivity and the Gut Microbiome in a Sex-dependent Manner 🔖 @AGA_CGH 👥@JacobsLabUCLA @LabusJS @TienDongMD @AndreaShin_GI @EmeranMayerMD @LinChangMD 🤝@NIH_ORWH @NIDDKgov 👉 https://t.co/fDJm2qfoKd
0
7
19
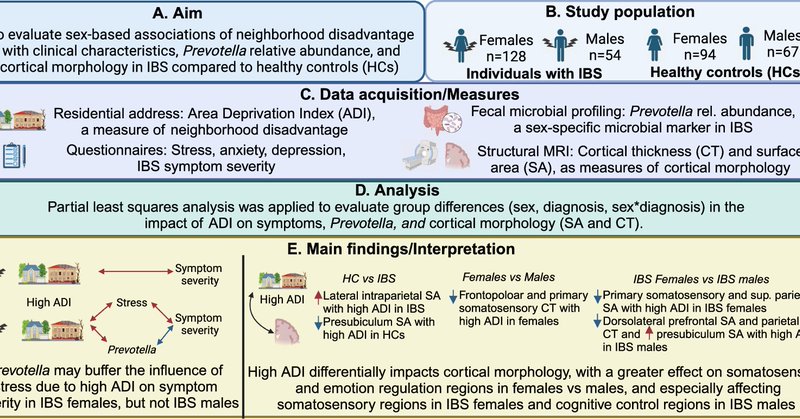
The choice of where you live affects IBS @ArpanaChurch, @LinChangMD, @EmeranMayerMD & colleagues found that living in areas with fewer healthy food options and less green space may link to worse gut symptoms: https://t.co/fPzt0M0957
link.springer.com
Biology of Sex Differences - Irritable bowel syndrome (IBS) is a stress-sensitive disorder that exhibits sex differences in brain–gut–microbiome interactions. Neighborhood disadvantage...
0
1
7
Live Biotherapeutics and postbiotics may benefit #IBS treatment says Dr. Andrea Shinn from @UCLA @LindaNguyenMD @LinChangMD @AmCollegeGastro course concludes #microbiome #DGBI
1
6
15
Impact of Short Duration FODMAP Restriction on Breath Gases and Gastrointestinal Symptoms Pathipati, et al. ➡️ https://t.co/UdJpG0cT5a
@mraonghus @claire_shortt @umfoodoc @LinChangMD @drkylestaller
1
12
23
Meet the newest team members driving excellence, innovation and impact at #UCLAGI! 🌟@AmirGhaffariMD 🌟Andrew Gregg, MD, PhD 🌟Brian Horwich, MD, MS (@Typical_Brian) 🌟Amanda J. Krause, MD 🌟@SarinaLoweMD 🌟Alex Nguyen, MD 🌟Mickeal Pugh, PhD
0
2
30
Inspiring to listen to this powerhouse panel at the Women in Neurogastroenterology & Motility Session at #ANMS2025 Amazing to hear these women share their experiences, reflections, and pearls led by @LindaNguyenMD & @LinChangMD (two of my role models in NeuroGI!) @ANMSociety
1
4
18
Excited about our paper investigating the impact of neighborhood in IBS: insights from brain gut microbiome alterations @UCLAGIHep @LinChangMD @AndreaShin_GI @EmeranMayerMD @UCLAHealth @dgsomucla @A_BioME #GoodmanLuskinMicrobiomeCenter
Study finds your neighborhood 🏘️matters for #IBS! Living in areas with fewer healthy food 🍲options & less green space 🌳 may link to worse 📉gut symptoms. Urban planning & lifestyle changes could make a difference! https://t.co/F0Cq6S9Iln
#PublicHealth #UrbanLiving
1
8
23
ANMS 2025 subgroup sessions are on the books! Don't miss the Women in Neurogastro sessions on August 8th from 5-6PM! @LindaNguyenMD @LinChangMD @NehaSantucciMD @AndreaShin_GI @ANMSociety @WalterChanMD @SaadJavedMD
Registration is open for the 2025 Annual Meeting, Young Investigator Forum, and Clinical Course. Make sure to take advantage of early bird registration pricing, which ends on May 19, 2025! https://t.co/sDNJjn0GPC
0
3
3
#CGH4ALL📣 💥 Check out the💡new data on #IBS care disparities in @AGA_CGH🔥! 🔗 https://t.co/jX3yUKKMUF Reported by @ifrahfatima
@AndreaShin_GI @LinChangMD
@ArpanaChurch @GregSayuk
@IBS_Maastricht @MelchiorChloe
@AndrewOngML @InclusiveIBS
@BrennanSpiegel @mgrover_gi
0
6
12
🧵 New RCT Alert! In a multicenter trial (n=280), 57.9% of #IBS-D patients responded to #acupuncture vs. 41.4% with #sham (RR 1.40, P = .008). Pain & diarrhea improved by week 3, effects sustained for 18 weeks. Safe, well-tolerated. https://t.co/kxUxxG3IR6
0
4
16
Thank you @AGA_CGH for highlighting our study!
Study examines the impact and interactions of race and gender on healthcare use and spending in #IBS ➡️ Learn more: https://t.co/O3AFqUKR84
@AndreaShin_GI
@LinChangMD
@ArpanaChurch
0
1
11
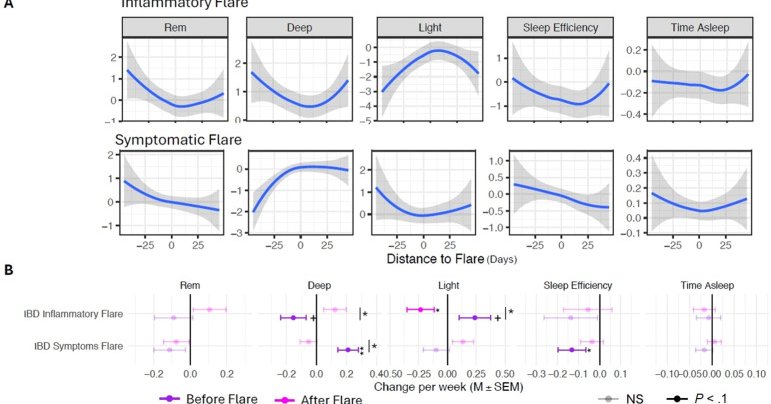
Excited to share our study using @Apple Watches, @fitbit & @ouraring in IBD. We found that inflammation-not symptoms-disrupts sleep. Sleep patterns change 45 days before/after flares, suggesting sleep could serve as an early signal of disease activity. 📄 https://t.co/5SqKeuJWWV
cghjournal.org
Poor sleep is associated with flares of inflammatory bowel disease (IBD). Studies often rely on subjective assessments of sleep and disease activity. Our aim is to use wearable devices to objectively...
3
6
25
Emerging technologies are poised to shift the field: ⚡Noninvasive neuromodulation 🧠Neural interfaces in gut & brain 🧬Microbiome-based diagnostics and therapeutics ⏳Real-time measures of vagal & spinal activity These tools could personalize treatment for obesity and DGBI.
1
3
6
What if 'gut feeling' was more than a metaphor, and the key to treating obesity and gastrointestinal disorders? This new commentary, born from the 2024 @NIDDKgov workshop on Interoceptive Contributions to Obesity & DGBI is now out in Gastroenterology: https://t.co/7cinsPS8Vg🧵👇
1
19
49
This #IBS researcher Dr. Singh had a lot of knowledge on #Foods and #IBS @GiHFoundation meeting! Rising star ⭐️ for sure!! #LFD #IBS markers @KateScarlata_RD @umfoodoc @LinChangMD @RomeGastroPsych
0
6
16
Grateful to the wise, compassionate, and ever-inspiring @ElisaBodenIBDMD for joining us as #UCLAGI Visiting Professor! 🌿 Her insights on sustainable careers in GI, feedback, and group CBT in #IBD empowered us all. 🙏💬🧠
3
6
28
Bloating vs Distention ▪️Bloating = subjective sensation ▪️Distension = objective sign ▪️Bloating feels like gas/pressure ▪️Distension measured by girth ▪️They can occur together ▪️They can also occur separately ▪️Eval both in GI complaints ▪️Different mechanisms ➡️ same sx
3
75
283