Madison Simons, PsyD
@DrMadisonSimons
Followers
528
Following
1K
Media
56
Statuses
652
GI psychologist at the Cleveland Clinic | Working in the intersection of digestion, nutrition, and psychology | Mom of 👦🏼👧🏼👶🏼 | runner
Joined March 2021
Hear from @GIdietitian, @DrV_IBD, and @DrMadisonSimons providing evidence-based nutrition strategies for patients with #IBD. Learn practical guidance on collaborating with dietitians and multidisciplinary teams to improve patient outcomes. Register ➡️ https://t.co/ACEMaU4xbD
0
9
16
She saw five specialists in two years. Gastroenterology. Neurology. Psychiatry. “Nothing’s wrong.” “Maybe it’s anxiety.” “It’s the weed.” She was throwing up weekly, bloated daily, and missing work. This isn’t rare. This is what it looks like when the system fails the complex.
32
44
450
The most common group of patients discharged from ERs in America today? Not chest pain. Not trauma. Not asthma. It’s the person writhing in pain, vomiting for hours, dehydrated, desperate, and told: “Your tests are fine. Follow up with GI.”
49
73
794
Excited to share our @IBDJournals publication on food fears in #IBD: what are the drivers of fear/avoidance, how can we best help patients with #diet liberalization? Read on for specific strategies for your practice! @DrMadisonSimons
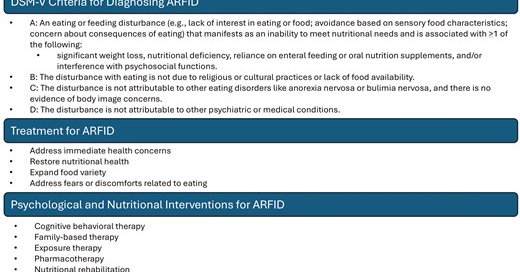
#ARFID
academic.oup.com
Abstract. Prior research has estimated the rates of avoidant/restrictive food intake disorder (ARFID) to be between 10% and 54% in patients with inflammato
4
7
34
Proud to share our new publication on food fear in IBD. We outline the neuroscience behind how fear of food develops in patients with GI symptoms and set the stage for a compassionate approach to reintroduction. https://t.co/0ygpn3GmN2... Thanks to @GIdietitian for initiating!
0
1
14
A 4week trial found that transcutaneous auricular vagus nerve stimulation (#taVNS) significantly improved constipation and abdominal pain in #IBS-C patients. Benefits include better rectal sensation, vagal activity, mental health, & gut microbiota balance. https://t.co/l9Sbv4S4yg
0
8
18
There are many reversible causes of bloating but abdominal distension to the point of looking pregnant is often refractory to simple treatments. Abdominophrenic dyssynergia (APD) is often implicated due to an abnormal viscerosomatic reflex, leading to an abnormal diabetic
3
12
29
@SKhalilMD @MountSinaiNYC We will have an article out soon in @DDS_Journal about current trends practices & attitudes of GI providers for endometriosis screening in pts with chronic GI symptoms! @IrisWangMD @DrMadisonSimons @drlauriekeefer Moving the needle slowly ….
0
1
7
For some good news and progress: yesterday I saw two patients referred from our GI team here for menstrual related GI symptoms and query Endo. Both have deep disease. Collaborations and connections work. #Endo @EndoWhat @EndoEICE @PelvicPainOrg @jjfitzgeraldMD @nancynursez637
3
3
20
🥗Check out this study where @DrMadisonSimons from the @ClevelandClinic and team explore the food related quality of life for patients experiencing organic GI conditions (like IBD, celiac sprue, and eosinophilic esophagitis. Read more on JHND early view: https://t.co/o87EqGfjil
0
2
3
If you treat patients with gastroparesis (or have it yourself), check out this nutrition guide by @KateScarlata_RD on how to navigate food/eating with gastroparesis! Diet change is your first line of treatment and then you stack others on top.
katescarlata.com
This 8-page educational handout covers a primer of gastroparesis with up-to-date clinical practice guidelines and tips for eating well while managing symptoms. The 4 key components of the nutritional...
1
1
6
Lastly, talk to your patients about how their symptoms affect their appetite, taste/smell of food, and fear around food/eating. This is especially prominent in patients with dyspeptic symptoms (nearly 50%) #ACG2024 @ClevelandClinic @Psylupe @EStaneffPsyD
0
2
8
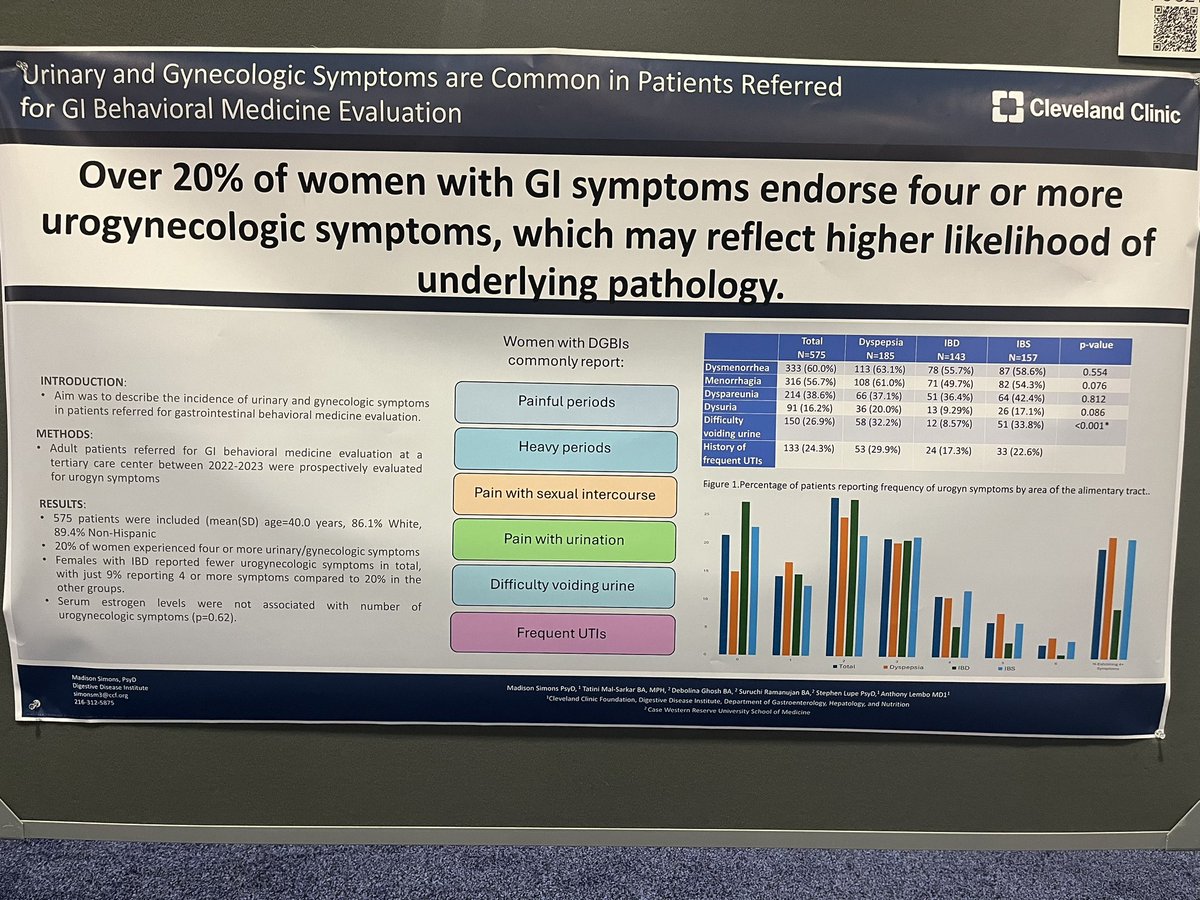
Why should you screen for endometriosis? 20% of patients with GI symptoms report 4 or more of these symptoms. This may reflect underlying urogyn pathology affecting the GI tract #ACG2024 @ClevelandClinic @Psylupe
2
7
23
In collaboration with @IrisWangMD @yuyingMD, we studied screening practices for endometriosis among GI providers. Most are not currently screening- ask your pts about: -painful periods -heavy periods 🩸 -painful sex -painful urination -frequent UTIs #ACG2024 @ClevelandClinic
0
6
14
#ACG2024 Poster session happening now- Honored to receive a presidential award for our research showing 2/3 of patients w/ autoimmune gastroparesis benefit from IVIG therapy ✨ Unfortunately, insurance is a significant barrier to receiving this life changing treatment…
2
3
13
Heart warming to see a full room- @BMoshiree speaks on #gastroparesis diagnostics/treatment based on most bothersome symptom. We need ⬆️ GP txs + well equipped providers to care for these patients! Proud to be part of @ClevelandClinic & our multidisciplinary GP team #ACG2024
0
4
21
Baby’s first #ACG2024 ✨ Looking forward to sharing our research on appetite factors, urogyn sx, endometriosis screening, and IVIG for gastroparesis. Come see what we’re doing and get a look at this amazing hair in the poster hall Sunday 3:30-7pm ❤️ @ClevelandClinic
1
1
19
More to come as we continue to study these constructs but appreciate the collaboration with @DoerflerBethany @DrKateTomasino @DrAnjaliPandit @AnthonyLemboMD
0
0
0
As always, I hope as providers we can help patients find flexibility around food and eating to decrease hypervigilance. That said, for so many pts with severe and prolonged postprandial responses, we often have to understand food behaviors through a lens of the brain in trauma.
1
0
1
We found patients who had seen an RD (specialized or general) had the lowest FRQOL. It is unknown whether these pts had low FRQOL prior to seeking RD intervention or if dietary interventions increased hypervigilance around food/eating.
1
0
0