Sanjeev Sethi
@SethiRenalPath
Followers
14K
Following
3K
Media
474
Statuses
2K
Professor, Pathology, Mayo Clinic, MN. 💯 clinical. Renal pathology. Use X to teach, clinical info changed=protect confidentiality. Love dogs. Views are my own.
Minnesota, USA
Joined January 2018
A very happy and proud moment for me. Our son Amit started medical school at the University of Minnesota Medical School- Primary Care education at its best. @umnmedschool
60
10
630
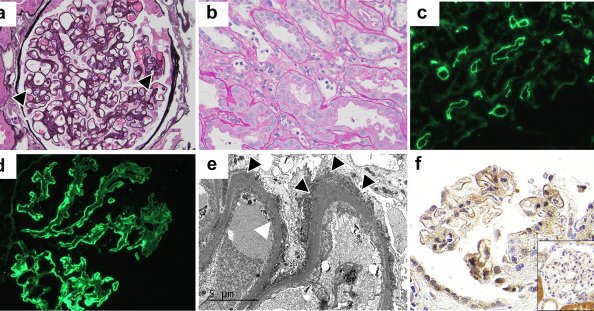
FAT1 is the target antigen in membranous nephropathy associated with-.1. Stem cell transplant (HSCT). 2. Antibody mediated rejection (ABMR) in allograft. In this paper we show a temporal ⬆️of FAT1 in MN with ABMR using protocol & for cause biopsies. 1/2.
kireports.org
Membranous nephropathy (MN) of the kidney allograft can represent recurrent, de novo, and very rarely, donor-derived disease. Despite its negative impact on allograft survival,1 our understanding of...
1
42
95
RT @NatRevNeph: Antigens in membranous nephropathy: discovery and clinical implications
nature.com
Nature Reviews Nephrology - Since the discovery of PLA2R, several target antigens associated with membranous nephropathy have been identified. This Review describes the distinct clinical...
0
36
0
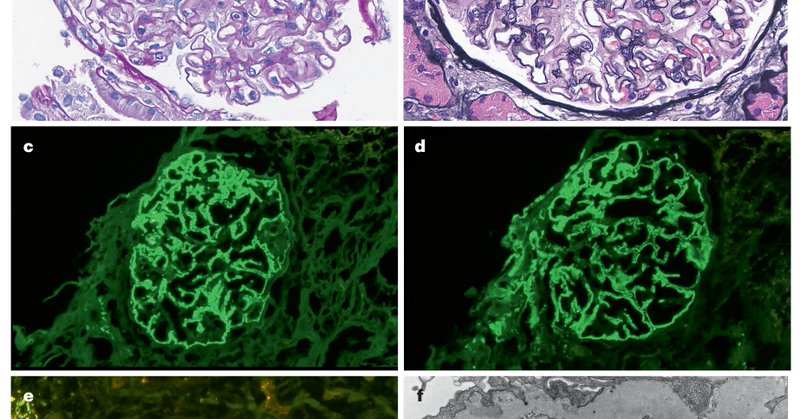
Membranous nephropathy has undergone a paradigm shift due to the discovery of unique MN antigens. MN has gone from idiopathic to ➡️ primary vs. secondary ➡️ where an antigen can be detected in ~80% of MN. This is a comprehensive review of each antigen.
nature.com
Nature Reviews Nephrology - Since the discovery of PLA2R, several target antigens associated with membranous nephropathy have been identified. This Review describes the distinct clinical...
6
89
206
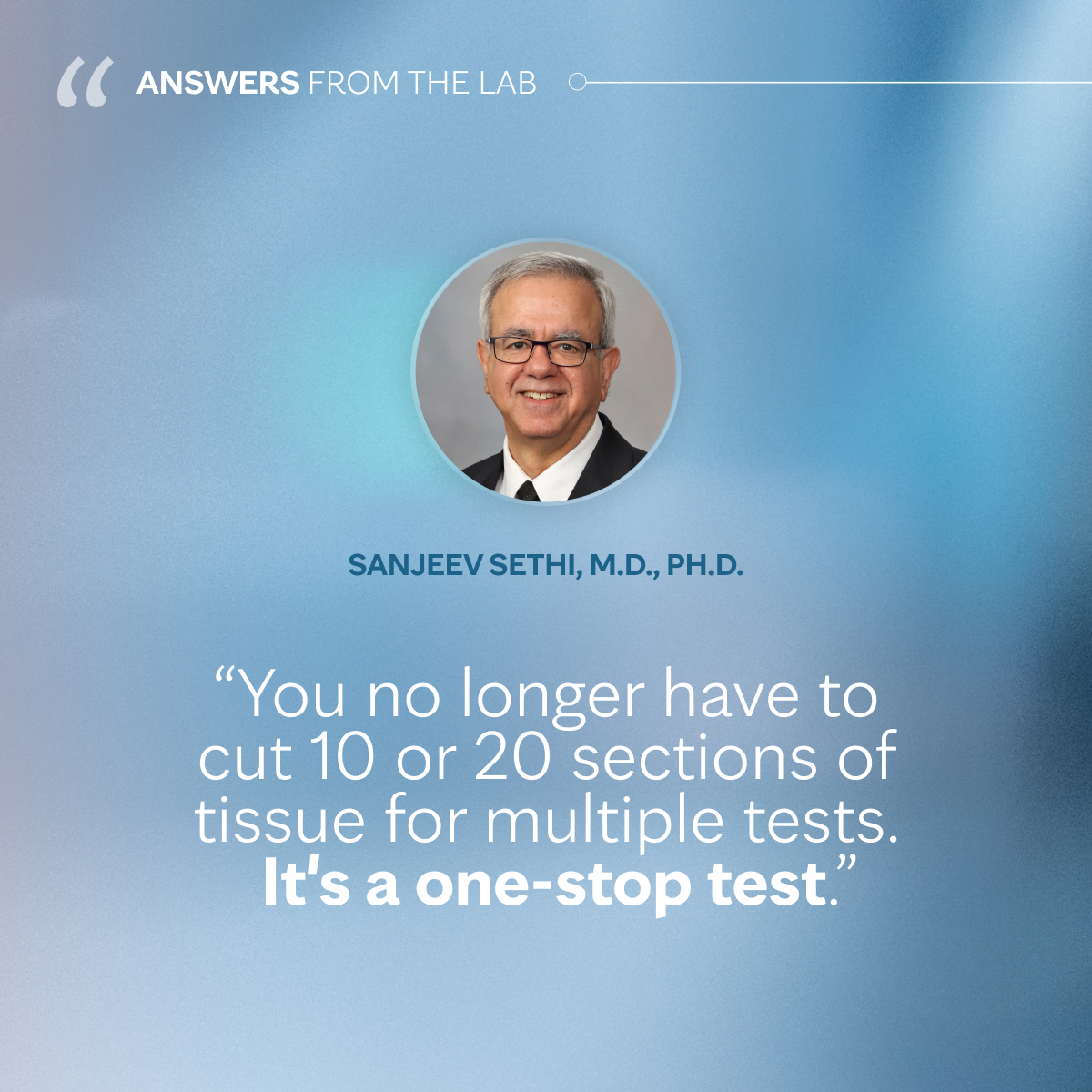
Laser microdissection and mass spectrometry (LMD/MS) is a sensitive one stop methodology for detecting large number of MN antigens. 3/3.
Mayo Clinic Laboratories' new mass spectrometry assay requires just one small tissue sample to identify 13 antigens known to cause membranous nephropathy. Learn more about this one-stop test. @SethiRenalPath.
0
2
11
Membranous nephropathy (MN) antigens from a single center in Portugal. Starting point=negative serum anti-PLA2R titer cases. We detected MN antigens: 3 PLA2R, 2 NELL1, & 1 each EXT1/EXT2, HTRA1, THSD7A. Antigens correlated with underlying disease. 1/2.
kireports.org
Membranous nephropathy (MN) is a rare autoimmune disease affecting individuals of all ages, standing as the primary cause of adult nephrotic syndrome and carrying significant disease burden.1
3
29
85
RT @mayocliniclabs: Mayo Clinic Laboratories' new mass spectrometry assay requires just one small tissue sample to identify 13 antigens kno….
0
20
0
RT @PepaSolerR: 📣📢 “𝟏𝐫𝐬𝐭 𝐌𝐚𝐲𝐨 𝐂𝐥𝐢𝐧𝐢𝐜 - 𝐕𝐚𝐥𝐥 𝐝’𝐇𝐞𝐛𝐫𝐨𝐧 𝐍𝐄𝐏𝐇𝐑𝐎𝐋𝐎𝐆𝐘 𝐔𝐏𝐃𝐀𝐓𝐄” save the dates 5-6 Sep Barcelona 2025. Register to mundicongres@mun….
0
28
0
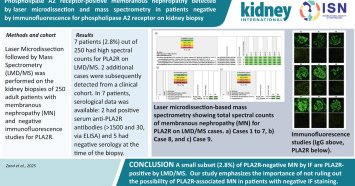
Sorry I accidentally deleted the original post while trying to answer some questions. I’m still a novice with X 😁. Take home message: small ~3% of PLA2R negative MN cases by routine IF are PLA2R positive by LMD/MS.
kidney-international.org
Membranous nephropathy (MN) is characterized by subepithelial deposition of immune complexes along the glomerular basement membrane. The muscle-type phospholipase A2 receptor (PLA2R) has been...
3
21
76
RT @andreaangioi: 🌍 ERA Congress 2025 – Vienna.🧠 Focus: Membranous Nephropathy. An inspiring session chaired by Ingeborg Bajema & Michael R….
0
12
0