Sam Tsimikas
@OxPL_apoB
Followers
2K
Following
22
Media
48
Statuses
234
All things OxPL, @Lpa_doc
San Diego, CA
Joined December 2018
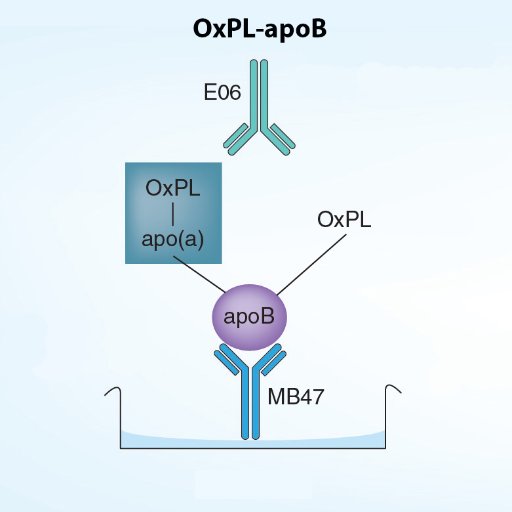
For those interested in research studies, OxPL-apoB and OxPL-apo(a) are now be available at Medpace. We will continue doing the tests @UCSanDiego for academic collaborations. For clinical care, OxPL-apoB is available @BostonHeartDX
0
1
2
We have a new, comprehensive review on oxidized phospholipids since last one in 2011. https://t.co/XuXsH6lZZ3 Covers pathophysiology, methodologies, evolution, clinical data, risk reclassification, therapy and more. I will be reviewing parts of this in the OxPL Sat AM Class
3
6
29
For those working on OxPL research and want/need antibody E06, there was a hiatus due to Avanti being bought out, but you can now buy E06 IgM through our collaborators at Millipore. https://t.co/TAtWOD07Po
0
1
2
No, Lp(a) is a risk factor, not a disease, therefore, it has no sxs until the disease starts (CAD, stroke, etc). That is why it is important to identify and treat early.
If a person with high Lp(a) of 219mnol/(88mg/dL) starts taking a PCSK9 inhibitor - will that person "feel" a difference? Given that person in already on a statin with cholesterol panel in range except high non-HDL @PeterAttiaMD @OxPL_apoB
2
0
6
Dr Constantinides was an MD/PhD pathologist. Being ahead of your time is good in retrospect, but not at that moment when you can't convince more people of the importance of your findings. Its that for many things in life, timing is a big part of succcess and progress....
0
0
0
Answers are in: 75% got it right- C. Note in the figure of a ruptured plaque how little apoB is present (noted by antibody MB47 that stains it) vs how many macrophages, OxPL (E06), Lp(a) (LPA4) and OxLDL (MDA2/IK17). Bottom line, inflamed lesions = ⏫ OxPL>OxLDL>Lp(a), ⏬ apoB
19/20 and the quiz: What is the correct statement: A- apoB accumulates as lesions progress B- Lp(a) diminishes as lesions progress C- OxPL accumulates and peaks at plaque rupture stage D- Answer please
0
2
6
20/20 Dr Constantinides was a: 1- Pathologist 2- Internist 3- Cardiologist 4- Cancer researcher
0
0
1
19/20 and the quiz: What is the correct statement: A- apoB accumulates as lesions progress B- Lp(a) diminishes as lesions progress C- OxPL accumulates and peaks at plaque rupture stage D- Answer please
1
1
1
18/20 In vivo evidence of OxPL in daily clinical practice is derived from studies evaluating the content of debris from distal protection devices in patients undergoing percutaneous interventions - nice case by @AHRavandi when he was a fellow with me- we are so proud of him!!
1
0
1
17/20 Interpretation: LDL/apoB is important in early lesions, but the ones that are clinically relevant and most associated with adverse events are ones cantain lots of OxPL and Lp(a)
1
1
0
16/20: OxPL were strongly present in late lesions in macrophage-rich areas, lipid pools, and the necrotic core, and most specifically associated with unstable/ruptured plaques. Apo(a) was present throughout early and late lesions, especially in macrophages and the necrotic core.
1
0
0
15/20 Although the presence of OxPL and apolipoprotein(a) increased in proportion to plaque progression and complexity, the patterns differed according to plaque type and plaque components.
1
1
0
14/20 In contrast, OxPL and apo(a) were present in 100% of foamy macrophages and were approximately 10 times more frequent in the shoulder region, fibrous cap, and necrotic core relative to apoB-100 immunostaining.
1
0
1
13/20: As lesions progress macrophages are primarily present in fibrous caps, shoulder areas and necrotic core. ApoB-100 was present in only 25% of macrophages and did not increase as lesions progressed and was rarely present in the shoulder region, fibrous cap, or necrotic core
1
0
0
12/20 We had the opportunity to work with her group and published a comprehensive paper on the presence of apoB, OxPL, Lp(a), and macrophages in each of these lesions. https://t.co/U8sfzqa6bR What is bottom line?
1
0
1
11/20 Dr Virmani and her group then re-classified the AHA classification of atherosclerotic lesions as: 1- Intimal thickening 2- Intimal xanthoma (fatty streak) 3- Pathological intimal thickening 4- Thick cap fibrous atheroma 5- Thin cap fibroatheroma 6- plaque rupture
1
0
1
10/20 The figure second down from the right is the classic vulnerable plaque: thin cap, partially obstructive, and inflamed at shoulder regions, leading to rupture and blood clot, first inside plaque, then occluding lumen
1
0
0
9/20 How do we classify human coronary atherosclerotic lesions? The original description of so-called vulnerable plaques were by Dr Constantinides in 1966. However, it was one of those observations, like many in life, whose importance was not appreciated for 30-40 years.
1
0
0
8/20 OxPL interact with specific receptors on a variety of vascular cells, such as CD36 and other scavenger receptors, CD14, TLR2 and TLR4 and LOX-1, to initiate a cascade of pro-inflammatory response
1
0
0
7/20 The interaction of OxPL with immune system results in acute/chronic inflammatory responses that can be detrimental to the host. The excessive and/or chronic generation of OxPL leads to protein degradation, cellular dysfunction, apoptosis, cell necrosis and tissue fibrosis
1
0
0

