Rotem Botvinik-Nezer
@rotembot
Followers
761
Following
1K
Media
15
Statuses
445
Senior Lecturer (Assistant Prof.) @HebrewU Psych. Studying belief updating and placebo with models and brains. Trying to make science more open & reproducible.
Joined January 2018
Now out @NatureComms! https://t.co/5AHORDIlLJ With @bogpetre (co-first) @torwager @Na_Friedman @fMRIstats @martaceko we show with fMRI & N=392 that placebo analgesia is driven by changes in brain systems related to affective & cognitive processes, not nociceptive pain processing
Our beliefs shape our response to treatment. Pretty amazing, right? @SIPSplacebo But do placebo effects operate via low-level perceptual or high-level cognitive and affective processes? Preprint w/ @bogpetre @martacek @fMRIstats @Na_Friedman @torwager
https://t.co/PHexnHYyJ3 🧵👇
2
17
58
And alongside that: we examined how expectations are formed from multi-value social cues, and how they shape both pain and visual perception. Integrating behavior, neuroimaging, and computational modeling.
growkudos.com
This study explores how our expectations influence what we feel and see. We asked participants to predict how painful or visually intense an upcoming stimulus would be based on cues that they...
Predictive processing models posit top-down influences of internal models on brain processing at multiple levels, including sensory processing. But they don't specify the details. How deep does predictive information penetrate into perception? What are the limits? New paper on
0
0
5
Read this #openaccess #PapersoftheWeek pick from @rotembot et al. and @NatureComms about placebo treatment’s effect on brain systems related to affective and cognitive processes, as well as its lack of evident effect on nociceptive pain https://t.co/be3vaGoSgk
#PRF
0
1
2
Read this #openaccess #PapersoftheWeek pick from @rotembot et al. and @NatureComms about placebo treatment’s effect on brain systems related to affective and cognitive processes, as well as its lack of evident effect on nociceptive pain https://t.co/WXKTUJ1cme
#PRF
0
2
4
0
2
5
The #Dartmouth Brain Imaging Center and Cluster on the #Neural Code are expanding! We have openings for permanent, high-level research staff positions: - DBIC Staff #fMRI #physicist - Neural Code Cluster Research Scientist/Research Asst Prof Please RT, and find me at OHBM!
5
47
66
🚨WP🚨 Conspiracy beliefs famously resist correction, right? WRONG: We show brief convos w GPT4 reduce conspiracy beliefs by ~20pp (d~1)! 🡆Tailored AI evidence rebut specific arguments offered by believers 🡆Effect lasts 2+mo 🡆Works on entrenched beliefs https://t.co/4VI0mzRqD9
44
225
708
It was a pleasure talking with @fMRI_today about analytical variability #narps
https://t.co/mQ9j8ZHanG, promoting open & reproducible science ( https://t.co/o0XcwCRyPG;
https://t.co/jXqMOxpmxx;
https://t.co/nOrjh2GXqn), placebo effects https://t.co/PHexnHYyJ3,
#OHBM, & much more!
nature.com
Nature - The results obtained by seventy different teams analysing the same functional magnetic resonance imaging dataset show substantial variation, highlighting the influence of analytical...
🎙 Join us in this Neurosalience episode with @rotembot and @fMRI_today, where they dive into the nuances of neuroimaging analysis—from the impact of shared data to the intriguing interplay between brain perception and pain. https://t.co/3jOyd11GN7
0
6
22
Excited to share our commentary led by the brilliant @JWeinrova (@notts_psych)!
0
3
16
** I am hiring a research assistant! ** Interested in mind-body treatments for chronic pain? Brain imaging studies of pain and emotion? Statistical methods and AI? Come join our team in beautiful Denver Colorado! Now accepting applications: https://t.co/N7oyMtqdmv please RT
1
13
22
After 5 years of collecting data on this project--the largest placebo neuroimaging study to date--it's wonderful to be able to take fMRI correlates of placebo analgesia to the next level of scale!
Our beliefs shape our response to treatment. Pretty amazing, right? @SIPSplacebo But do placebo effects operate via low-level perceptual or high-level cognitive and affective processes? Preprint w/ @bogpetre @martacek @fMRIstats @Na_Friedman @torwager
https://t.co/PHexnHYyJ3 🧵👇
2
17
89
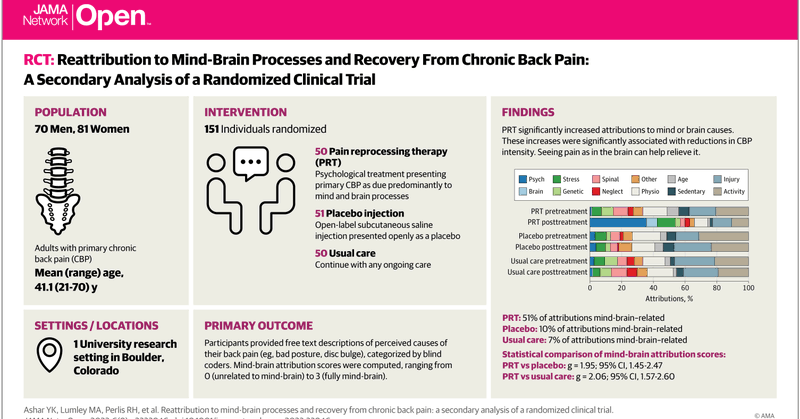
Seeing chronic back pain as due to the mind or brain can help heal it. Check out our paper published today in JAMA Network Open, using natural language methods to study patients' **pain attributions** https://t.co/v4519JHXKb Tweet thread: 1/n
jamanetwork.com
This secondary analysis of a randomized clinical trial examines whether patient reattribution of primary chronic back pain to brain- or mind-related causes is associated with pain relief in pain...
10
30
123
individual differences, surprising reversed neural placebo-induced responses in the transfer condition, and more. As always, data and code are publicly shared, take a look and use them @openscience! Data @OpenNeuroOrg
https://t.co/Fw1wZ1ZjAX, code https://t.co/VY76SSa4qz (end)
github.com
Code, data and figures for the paper on placebo effects based on the Paingen dataset - rotemb9/paingen-placebo-fmri-paper
0
2
16
placebos mainly operate via higher-level processes, and transfer between pain modalities. These findings open new directions for how to harness placebo effects and placebo-like processes to improve clinical care. Read our preprint for more https://t.co/PHexnHYyJ3, including (10)
1
0
5
Decreased activity in a second validated a priori neuromarker, the Stimulus Intensity Independent Pain Signature (SIIPS), along with several pre-registered higher-level brain regions inc. prefrontal and striatal regions. This means that, at least in experimental settings, (9)
1
0
3
In fact, Bayes Factor analyses provided strong evidence in favor of the null hypothesis of no placebo effect in these regions and signature. Instead of modulation of low-level perceptual processes, we found modulation of higher-level processes: (8)
1
0
4
(because thermal and mechanical pain diverge in early channels). But what about the brain? The placebo treatment didn't decrease activity in the Neurologic Pain Signature (NPS), the most validated nociceptive pain neuromarker, and in a series of preregistered nociceptive ROIs (7)
1
1
5
Participants were conditioned with the creams and thermal painful stimuli, but the placebo effect also transferred to a second, unconditioned pain modality- mechanical (and was as strong in this transfer condition!), suggesting involvement of higher-level processes (6)
1
0
5
First, the placebo manipulation (inc. suggestion & conditioning) worked well: Participants reported less pain when they believed they were treated with an analgesic vs. a control cream (although both creams were in fact identical!) (5)
1
0
4
small samples, and meta-analyses showed that these effects are often small. So, we revisited this fundamental question with a combination of the largest placebo fMRI sample to date (N=392!), pre-registered analyses, and validated fMRI-based multivariate neuromarkers for pain. (4)
1
0
8