ME/CFS Science
@mecfsskeptic
Followers
4K
Following
19K
Media
599
Statuses
8K
In-depth analysis of research on myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS).
Joined October 2016
David Tuller has played an important role in highlighting the problems with trials of CBT and graded exercise therapy for ME/CFS, such as the PACE trial. You can support his work using the link below.
Berkeley's fall crowdfunder for Trial By Error has launched: https://t.co/McAr649EVr
0
8
58
Does anyone know where these formula's for the heart rate limit come from? Are they based on experience or is there some physiological justification for them? @PhysiosForME @4Workwell
@SamanSarraf They used different formulas, patients had to option to choose: For the Garmin wristband: 1) (208–70% of age) × 0.55 2) Resting HR plus 15 bpm For the Visible armband: 3) (220-Age) × 0.6 Option 2 is based on the Workwell Foundation advice and more restrictive (lower limit)
1
0
11
Berkeley's fall crowdfunder for Trial By Error has launched: https://t.co/McAr649EVr
crowdfund.berkeley.edu
Help UC Berkeley raise $68,000 for the project: David Tuller's Trial by Error Fall 2025. Your gift will make a difference!
3
17
43
10) Link to the paper: Clague-Baker 2025. Pacing with a heart rate monitor for people with myalgic encephalomyelitis/chronic fatigue syndrome and long COVID: a feasibility study. https://t.co/y8W5QyuxFA
tandfonline.com
People living with ME/CFS and LC frequently live with post-exertional malaise (PEM), which is associated with impairments in aerobic metabolism. They often use pacing with a heart rate monitor (HRM...
1
2
34
9) Some are concerned that pacing may lead to decreased activity levels but the accelerometer data showed that it largely remained the same in both the intervention and control group. (only) 1 Long Covid patient reported anxiety from monitoring their HR limit with alarms.
1
0
25
8 ) There were also no discernible changes in the blood pressure, heart rate, and oxygen saturation measures before and after the intervention. Both the control (3.7–2.7) and intervention groups (3.7–2.9) showed decreased levels of lactate.
2
0
17
7) The outcome measures are hard to interpret because the authors don't report variability or statistical tests. But it seems that there weren't notable differences between groups in for example fatigue or physical functioning.
1
1
15
6) The results: the trial and its many measurements were doable, there weren't many dropouts or issues. Some participants did find it hard to fill in a PEM diary for 2 months and five ME/CFS patients didn't tolerate the standing test.
1
0
21
5) All these measurements and interventions were carried out in the participants’ homes. Patients were mainly recruited from social media but it was difficult to find sufficient Long Covid participants (as many were already using a heart rate monitor).
1
0
17
4) The most fascinating aspect of this trial is that it measured multiple objective outcomes: a 10-minute standing test (for POTS), an accelerometer for activity levels, a FirstBeat bodyguard to measure physiological stress and recovery, and a device that measured lactate.
2
0
26
3) The device gave an alarm notification when patients exceeded their chosen heart rate limit. Patients in the control group got pacing sessions but without the use of a heart rate monitor. The trial lasted for 8 weeks.
1
0
19
2) Pacing is a way to manage activities to avoid post-exertional malaise. Patients in the intervention group got a wrist-based Garmin device or an arm-based strap with the Visible app. Their heart rate limit was calculated using personalised formulas such as: (220-Age) × 0.6
2
0
19
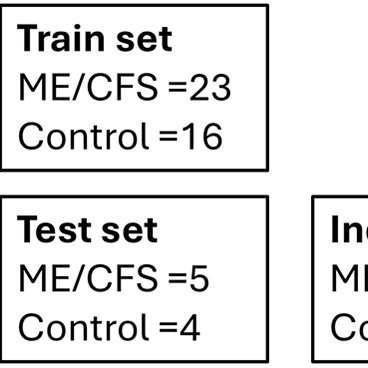
1) The Physios for ME team published a randomized trial on pacing with a heart rate monitor. It included 32 patients with ME/CFS and 15 with Long Covid. A brief breakdown of the main results 🧵
6
23
113
RT @RorPreston: One thing that I would note that is encouraging about this study is that it was lead by a private company - Oxford BioDynam…
0
3
0
9) The study is question is: Hunter et al. 2025. Development and validation of bloodbased diagnostic biomarkers for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) using EpiSwitch® 3-dimensional genomic regulatory immuno-genetic profiling. https://t.co/8ZBlTmBG7o
translational-medicine.biomedcentral.com
1
3
26
8 ) The epigenetic test might be interesting but it needs to be done on larger and better samples to avoid confounding by sex, activity levels, databases, etc. We aren't the only ones with reservations, see these comments by experts on the SMC: https://t.co/Wl538QF4QO
1
1
30
7) The pathway that stood out the most involved Interleukin-2 (IL-2). The authors suggest that this can be used to subgroup patients and they propose twelve therapies that target this pathway (some such as Rituximab and Rapamycin have already been trialled in ME/CFS).
1
2
32
6) The researchers highlight that their results "suggest a strong immunological component in ME/CFS pathology." They found overlap with pathways implicated in multiple sclerosis, rheumatoid arthritis and other chronic inflammatory disorders.
1
1
31
5) The model had an accuracy of 96%: it correctly classified 22 out of 23 ME/CFS patients and 44 out of 46 controls. ME/CFS, however, is likely a heterogenous syndrome so 100% accuracy should not be the main goal of such a test (it should be to find relevant pathology).
2
1
28