Mahsa Dolatshahi
@MahsaDolatshah1
Followers
2K
Following
6K
Media
53
Statuses
571
PGY1 resident @MissouriBaptist || Incoming research track radiology resident @WashUMedMIR class of 2030 || MD-MPH Graduate @TehUofMed
St Louis, MO
Joined March 2021
9/9 Take-home: C-FLAIR addresses a common diagnostic pitfall: skull-base FLAIR hyperintensity that mimics pathology. ✨A small sequence-level change → clearer images, fewer false positives, stable lesion visibility. @VChernyakMD @RITEditor @DrLindaMoy @ProfVickyGoh @chemshift1
1
0
1
8/9 Pulse is shorter (3.82 ms vs 17.16 ms) and Specific Absorption Rate (SAR) increase is modest (~14%) ⚡ No need for per-subject calibration. Scales cleanly to routine clinical use.
1
0
0
7/9 Workflow impact: None ⏱ Same scan time 🔧Same reconstruction 🏥Same hardware The only difference is swapping the inversion pulse in the sequence library. No operational friction.
1
0
0
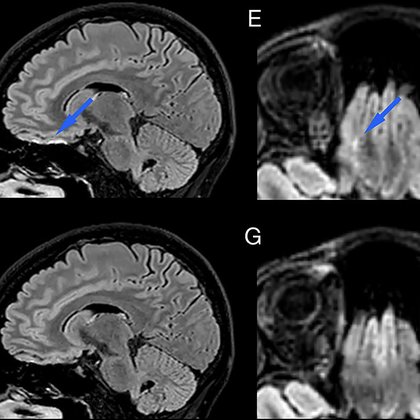
6/9 👥 Human imaging (n = 14 across multiple conditions): C-FLAIR removed skull-base hyperintensity artifacts while preserving lesion visibility in MS and white matter disease ✅ 🩻Key Clinical Point: • SNR unchanged • CNR unchanged
1
0
0
5/9 🧪 Phantom test: Standard FLAIR → large bright artifact near induced inhomogeneity C-FLAIR → signal properly suppressed throughout This demonstrates the core mechanism clearly.
1
0
0
4/9 The authors designed a new inversion pulse (C-FLAIR) using optimal control theory — basically designing the pulse to remain stable across a wide range of field conditions 🧠🔧 No extra hardware. No parallel transmit. Just a better inversion pulse.
1
0
0
3/9 This is especially noticeable at 3T 🎛️ Skull base, sinuses, and temporal bone regions are notorious for off-resonance and RF variation → where FLAIR is often least trustworthy. Here, the B, F images are acquired without T2-preparation to better expose the FLAIR artifact.
1
0
0
2/9 What is the issue? FLAIR suppresses CSF using an inversion pulse 💧 But when field inhomogeneity disrupts that inversion, CSF doesn’t fully null → bright signal → false-positive lesions ⚠️
1
0
0
1/9 Can we fix skull-base FLAIR artifacts just by changing the inversion pulse—without changing scan time or hardware? Turns out - yes ✨ A new paper in @radiology_rsna explores this idea: https://t.co/9TGwgbBGc7
#RadInTraining @RITEditor @RadiologyEditor
pubs.rsna.org
Robust inversion in fluid-attenuated inversion recovery reduced artifacts in brain MRI that mimic hyperintense white matter lesions.
1
0
1
9/ 🧩 Bottom line: Measuring shades of gray on CT — as a marker of early infarct water uptake — may be the next step toward precision stroke care. #Stroke #Radiology #Thrombectomy
@VChernyakMD @RITEditor @DrLindaMoy @ProfVickyGoh @chemshift1
0
0
0
8/ Clinical takeaway: 📊 NWU could become a fast, standardized biomarker for stroke triage, especially in centers without perfusion imaging. Low NWU = treat aggressively. High NWU = consider futility or individualize.
1
0
1
7/ Safety check ✅ Thrombectomy did not increase hemorrhage risk, even in patients with high NWU. So NWU shouldn’t replace current selection criteria — it should refine them. Think of it as a guide, not a gate for thrombectomy decisions.
1
0
0
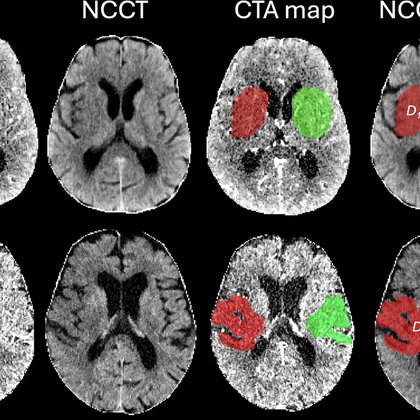
6/ Translation of these findings: CT doesn’t just show infarct size — it also shows infarct quality. 🧠 Quantifying NWU helps distinguish salvageable from unsalvageable brain tissue in low ASPECTS stroke.
1
0
0
5/ Patients with low NWU (<15%) had a clear benefit from thrombectomy → higher chance of walking independently at 90 days. Those with high NWU (≥15%) showed no added benefit over medical therapy.
1
0
0
4/ Higher NWU predicted worse outcomes (OR 1.11, P<.001). Thrombectomy improved overall outcomes (OR 0.33, P<.001). ⚡Key finding: Patients with lower NWU benefited most from thrombectomy. NWU does not just predict who does worse. It predicts who benefits most from thrombectomy.
1
0
0
3/ What’s NWU? It quantifies early brain edema from CT density differences between infarcted and healthy tissue. High NWU = more edema = more irreversible damage. 📉
1
0
0
2/ Background: Recent trials show thrombectomy helps some patients with large infarcts, but not all. How can we tell who truly benefits? That’s where NWU comes in — a CT measure of tissue hypoattenuation (water content = edema). 💧
1
0
0
1/ 🚨 New in @Radiology_RSNA: Quantitative net water uptake (NWU) on CT predicts who benefits most from thrombectomy in large-core stroke: secondary analysis of the TENSION trial (n=207). 🧠💉 https://t.co/alLg6TE56L
#RadInTraining @RITEditor @Radiology_Editor
pubs.rsna.org
Early infarct net water uptake at admission CT modified the treatment effect of endovascular thrombectomy (EVT) on functional outcomes and may help identify patients with a large infarct core who b...
1
3
16
🚨📈 CT use in the emergency department has nearly doubled in the past decade among Medicare patients. New @Radiology_RSNA study breaks down ED imaging trends from 2013–2023. 🧵on what’s driving the growth ⬇️ #RadInTraining #TWEETORIAL @radiology_rsna @RITEditor @VChernyakMD
1
11
18
📢 NAIRS Webinar Series We are excited to invite you to: Navigating the Radiology Residency Match: Interview Success Strategies 🗓 October 2, 2025 | ⏰ 8–9 PM ET https://t.co/oEE2dXcfnd
#Radiology #ResidencyMatch #NAIRS #Match2026 #RadRes
2
10
44