Ashley Miller
@icmteaching
Followers
9K
Following
18K
Media
447
Statuses
6K
#zentensivist #FUSIC Haemodynamics National Lead. ICS trustee. BSE level 2. BJJ ⬛️⬛️🟥⬛️ @Turningthe_Tide. No politics, just #foamed #pocus #haemodynamics
United Kingdom
Joined December 2015
Pinned: Cardiovascular Physiology Hub Discovering physiology together: untangling the concepts most often misunderstood at the bedside. Foundations – Starling’s law as servo-control https://t.co/dYJMFYH2nk – Cardiac output & Anderson’s model https://t.co/1yPzedaTtZ – Preload
1/ Most people think the heart drives circulation. But what if that’s backwards? Anderson’s model flips the whole idea of cardiac output on its head — and it changes how you think about fluid, flow, and failure. 🧵👇 #physiology #FOAMed #MedTwitter #criticalCare #cardiacOutput
2
57
158
Blast from the past. I wrote this 10 years ago. Here’s the correct link 😉
bjaed.org
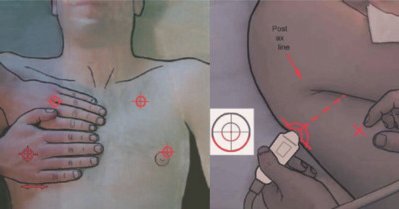
Critically ill patients need rapid access to accurate and reproducible imaging techniques to diagnose pathology, implement, and monitor treatment. Point-of-care ultrasound (US) has become firmly...
🖼️ The “seashore sign” vs “stratosphere sign” and B-lines can help distinguish: • pneumothorax • interstitial syndromes (pulmonary oedema, pneumonitis, fibrosis) POCUS becomes a bedside game-changer for pregnant patients with dyspnoea. 🔍🫁 Read more: https://t.co/mxQP57qVCQ
0
4
23
Sadly, we are starting to see it begin to bite. I am interviewing some experts tonight about the Influenza storm approaching. Podcast to be released very soon…. More episodes here: https://t.co/iQpdtAAt0o
#ecmo #influenza @ICS_updates @Zudin_P @RCoANews @Assoc_Anaes @yourICM
0
2
10
🏥 Health policy fight heats up on Capitol Hill Republicans explore options to fix scandal-ridden Obamacare subsidies while Democrats demand extension of broken program losing billions to fraud Do Dems want a policy win or a political fight?
1
6
23
Love this
@icmteaching @PulmCrit @kidney_boy Sometimes when I have a patient receiving albumin + Lasix (for days) from other attendings, I tell the nurses to add "albumin" in the list of "allergies"
3
3
20
Why you cannot be oedematous and hypovolaemic at steady state 👇 1/ “Puffy but intravascularly dry?” A common phrase on the wards – and one of the most persistent myths in IV fluid therapy. Oedema and hypovolaemia come from opposite pressure states. They cannot coexist once the
2
35
112
What haemodynamic / fluid physiology do you want me to post about? #FOAMed #physiology #haemodynamics #MedX
11
2
17
Jamie Dimon just launched a strategic council to secure America’s critical minerals future — backed by a $1.5 TRILLION “American Resiliency” commitment from JPMorgan. The all-star advisory group (chaired initially by Dimon himself): Jeff Bezos (Amazon) Michael Dell (Dell)
0
8
17
🎧 This one was an absolute hoot!! Take a 👂 https://t.co/DRlRF3oXru In this episode, we talk through ICM’s failings, future, bloopers and much more….added banter (It’s Mervyn, so obviously!) We have loads more coming your way in 2026. - Vets, Pets and ICU - How to
1
5
14
My friend Keith was recently diagnosed with an inoperable brain tumor. He is a MASSIVE Christmas music fan (@MichaelBuble ) He wrote and recorded an amazingly catchy Christmas song that he is trying to get covered as a legacy piece for his family ( recording below👇) Please
2
28
45
Very cool
(1/9) Academic writing in 2025 is still broken. Word. ChatGPT. Reference managers. Formatting. Reviewer #2. Copy paste. We built a better workflow. Introducing Livewrite, your new AI research assistant that runs directly inside Microsoft Word.
0
2
10
Good point. That interpretation of ALBIOS commonly comes up. I think it'sImportant to clarify what the trial actually showed (and didn’t show), because this misunderstanding drives a lot of albumin use. The “benefit” in the ALBIOS shock/MODS subgroup only appeared in post-hoc,
@icmteaching @iceman_ex Agree, in the heterogeneous ALBIOSIS population routine supplementation didn't benefit but it did in the more shocked/MODS subgroup (usual caveats). Presume higher shock burden had greater glycocalyx shedding/did benefit. HAS may have a role but need to define population better
2
3
15
There’s a hypothesis that albumin “protects” the glycocalyx but the evidence is extremely thin, and almost all of it is in vitro. Cultured endothelial cells shed their glycocalyx in protein-free media, and adding albumin back restores some features, but this doesn’t translate to
@icmteaching Is albumin glycocalyx friendly? Does it have a glycocalyx protective effect especially in hyperinflammatory states like sepsis?
5
11
49
Start here ⬇️ https://t.co/SU82nYsvbr
🧵 Albumin in Critical Care: 70 Years, 700 Papers… Zero Benefit 1/ Albumin is the most studied fluid in critical care. Decades of trials. Endless meta-analyses. And yet – not a single clinically meaningful benefit. Here’s why the entire theory collapses once you understand
1
3
11
13/ Summary Albumin: • does not treat oedema • does not restore intravascular volume (beyond minutes) • does not improve outcomes • leaks rapidly • suppresses synthesis • costs a fortune • is mechanistically incoherent with Extended Starling physiology 👉 70 years. 700
4
4
45
12/ The cirrhosis/paracentesis exception Post-paracentesis instability isn’t “hypovolaemia” Here the physiology is different: • sudden ↓ intra-abdominal pressure • sudden ↑ venous capacitance • transient ↓ Pms and ↓ venous return Hyperoncotic albumin provides a
3
3
39
11/ Trials confirm the physiology SAFE, ALBIOS, EARSS, SWIPE...etc: • no survival benefit • no organ failure benefit • no oedema benefit • no haemodynamic advantage • subgroup signals that never replicate decades of albumin trials → zero clinically meaningful effect.
2
2
29
10/ Why albumin doesn’t fix oedema Oedema is driven by: • ↑ Pc • ↑ permeability • ↓ Pi • lymphatic overload • excess ECF volume Albumin fixes none of these. And because it rapidly leaks, it can make oedema worse.
2
5
31
9/ Albumin leaks more when the glycocalyx is injured Fleck’s group demonstrated: • TER (albumin escape rate) doubles in critical illness • Hypoalbuminaemia is driven by accelerated escape, not loss • Infused albumin escapes faster than endogenous Giving albumin into a leaky
3
4
28
8/ Hypoalbuminaemia is a marker, not a deficit Low albumin in critical illness reflects: • oxidative stress • redistribution • accelerated transcapillary escape • dilution • decreased synthesis COP remains near-normal because acute-phase proteins rise. And importantly:
2
3
33
7/ Analbuminaemia: the knockout blow People born with virtually zero albumin: • are not chronically oedematous • maintain normal interstitial volume • only develop oedema when fluid-overloaded 👉 Oedema is a problem of ECF excess and high Pc – not hypoalbuminaemia. This
3
12
57