TheSpineJEditor
@TSJ_Editor
Followers
970
Following
95
Media
100
Statuses
367
Joined December 2018
This group was also older and more levels fused than the late revision group. 2/2.
thespinejournalonline.com
Adjacent segment degeneration (ASD) following lumbar fusion operation is common and can occur at varying timepoints after index surgery. An early revision operation for ASD, however, signifies a...
0
1
3
What’s trending down? MVAs, GSWs, sports/recreation injuries, and SCI’s. @UMmedschool .2/2
thespinejournalonline.com
Traumatic spinal injuries (TSI) are associated with high morbidity, mortality, and resource utilization. The epidemiology of TSI varies greatly across different countries and regions and is impacted...
0
1
3
Other data are reaffirming what we already knew—there was no incidence of delayed spinal instability. 2/2
thespinejournalonline.com
Gunshot wounds (GSWs) to the vertebral column represent an important cause of morbidity and mortality in the United States, constituting approximately 20% of all spinal injuries. The management of...
0
2
4
Okay, so I said it was rare to see articles on GSWs to the spine a while back. Well, here’s another one. Santangelo et al did a demographical update (which has not been done in a long time). Unfortunately, young black males are still the most affected. @URNeurosurgery 1/2
1
2
4
. in indolent conditions like pseudos and axial back pain. Read it and learn. 2/2
thespinejournalonline.com
Cutibacterium acnes (C. acnes) previously named Propionibacterium acnes (P. acnes) has been increasingly recognized by spine surgeons as a cause of indolent postsurgical spinal infection. Patients...
0
1
2
“Isn’t that cuti!” Not really, if we’re talking about Cutibacterium acnes. It might also be called, “The bacteria formerly known as P. acnes” (sorry Prince). Baroudi et al gave us a very thorough overview of C. acnes and its potential involvement . 1/2 @BrownMedicine.
1
1
2
Sure, variability is expected, but 30% of fellows did fewer than 250 cases. Is it enough? If more is better, then there’s work to be done. 2/2.
thespinejournalonline.com
There has been increasing scrutiny on the standardization of surgical training in the US.
0
1
2
“How many cases do your fellows do?” It’s one of the first questions candidates ask about a program. Is there a magic number? Silvestre et al assessed the number and kinds of cases done by spine fellows in the US. @MUSC_COM
1
1
3
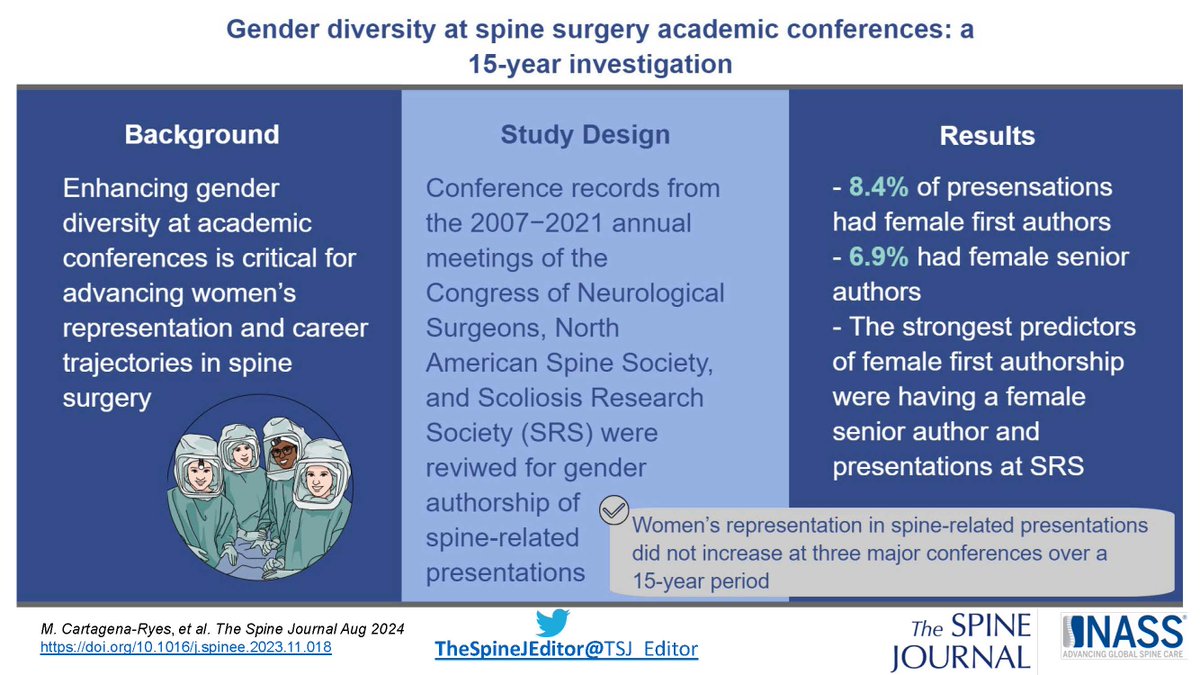
Cartagena-Reyes et al found no increase in women’s representation at 3 major meetings over 15 years. This is discussed in great detail, both about women and URIMs. In short, we need to be intentional and think outside our usual circles. @HopkinsMedicine
0
1
2
While blacks had higher chance of adverse events, reop, and non-home discharge after inpatient surgery, this was not the case with outpatient surgery compared to Whites. However, readmissions were still higher. 2/2
thespinejournalonline.com
Racial disparities in spine surgery have been thoroughly documented in the inpatient (IP) setting. However, despite an increasing proportion of procedures being performed as same-day surgeries,...
0
1
1
In world where inequities and health care disparities have infiltrated all corners of our world, it’s interesting to find outpatient spine surgery may be less disparate, per this paper by Amen et al. @HSpecialSurgery 1/2
1
1
1
I’m digging it—more objective functional outcome measures. A Danish group had patients with lumbar stenosis wear a thigh accelerometer for 7 days. Not too surprising, controls walked for continuous periods of moderate length than pts w/stenosis.
thespinejournalonline.com
One of the primary goals of treatments received by individuals with lumbar spinal stenosis with neurogenic claudication is to improve walking ability. Thus, a thorough and valid assessment of walking...
0
1
1
Using their parameters, they achieved 100% sensitivity and 92% specificity. I don’t know if I’m ready to give up my CT, but it’s compelling. 2/2.
thespinejournalonline.com
The disease of ossification of the posterior longitudinal ligament (OPLL) in the cervical spine was first reported by Key in 1838 [1]. Surgery for cervical OPLL accounts for about 5% of all cervical...
0
1
1
Take home points: VBQ (on MRI) and HU (on CT) can work to predict some important things—fracture, construct failure. So if you didn’t get the DEXA, use what you have. It may save you some trouble. 2/2.
thespinejournalonline.com
Low bone mineral density (BMD) can predispose to vertebral body compression fractures and postoperative instrumentation failure. DEXA is considered the gold standard for measurement of BMD, however...
1
1
2
I hate self-promotion but take a look at the nice review by Agaronnik et al about using MRI and CT for opportunistic bone density measurement. There was some much data out there (and continues to come), I f-igured it was time to synthesize it. 1/2 @harvardmed
1
1
1
It was 150% higher if given 61-120 minutes before incision. Wow—time to change the standard. 2/2.
thespinejournalonline.com
Surgical site infections (SSI) are one of the common complications following spinal fusion surgery. Unfortunately, several studies had shown conflicting results regarding optimal timing of surgical...
0
1
1