Kiran Rikhraj
@KiranRikhraj
Followers
975
Following
742
Media
66
Statuses
305
Intensivist in training, Critical Care Ultrasound fellow, EM doc
Joined August 2015
Head over to to hear more fantastic webinars from this all star crew!!.
hcprounds.com
Hemodynamics, Congestion, and Perfusion rounds led by Dr. Ross Prager and Dr. Eduardo Argaiz explores the cutting edge of phenotyped resuscitation.
0
0
6
What a fantastic #HCP webinar by @ross_prager @ArgaizR and @FH_Verbrugge on mastering diuresis. A few of the many things I learned and need to read up on below!
1
12
51
Back to basics! I am starting a new series of videos focusing on mastering basic #POCUS concepts. Starting off with honing your ability to obtain the 4 basic cardiac views and steps on how to obtain additional/advanced views. Please give it a watch: .
2
45
160
Incredibly informative and helpful thread. A must read for all resuscitationists!.
15. 🛑 That’s why it’s a mistake to “fill the heart to improve function.”.Distending the ventricle in search of better output often worsens failure (increases wall stress, oxygen demand, ventricular interdependency).You're stretching a failing system - not supporting a healthy.
1
1
6
Twitter friends: when deciding whether to tap a pleural effusion, what are the things you look at on #POCUS to determine if the effusion is safe to tap? . Poll below 👇
6
10
65
@NephroP @FH_Verbrugge @ArgaizR @EMNerd_ @CPSolvers @AllisonRBond @AndromedaShock (11/11) You need a team you can rely on and trust when working on something like #HR25. I am so thankful for @ThinkingCC @ross_prager @G2Disrupt @katiewiskar @AmyDhillon and @JasmineLam. Excited to start working on #HR26!.
2
2
20
@NephroP @FH_Verbrugge @ArgaizR @EMNerd_ @CPSolvers @AllisonRBond (10/11) Pay attention to how quickly Capillary Refill Time normalizes in septic shock resuscitation. @AndromedaShock pearl: Rapid normalization of CRT may reflect preserved macro- to micro-circulation coupling while failure to improve CRT is associated with increased mortality.
1
6
24
@NephroP @FH_Verbrugge @ArgaizR @EMNerd_ @CPSolvers (9/11) Think about your antibiotic routes more carefully @AllisonRBond shared her Top 10 Infectious Disease Pearls reminding us that not all antibiotics need to be given through an IV, even in bacteremic patients!
2
3
17
@NephroP @FH_Verbrugge @ArgaizR @EMNerd_ (8/11) Experience is not the same as expertise. @CPSolvers pearl: We should not be reflecting on a case for 20 hours over the course of 1 day but instead, think about the case for 1 hour every day for 20 days. Consistency matters!
1
1
16
@NephroP @FH_Verbrugge @ArgaizR (7/11) Pay attention to your patient's Minute Ventilation and their PaCO2. As @EMNerd_ cleverly described, the more dead space you have, the higher the MV you need to maintain a normal CO2. This increases a patient's respiratory workload and can drive weaning failure.
1
1
17
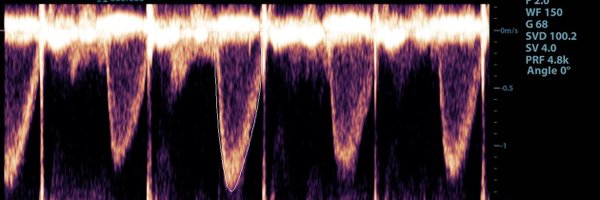
@NephroP @FH_Verbrugge (6/11) Key pearl from @ArgaizR on intrarenal vein doppler: Systolic-only flow in the IRV is an indication of pericardial disease. This needs to be interpreted VERY differently to diastolic-only flow (often due to more "classic" causes of congestion eg. TR, PE, volume overload)
1
2
20
@NephroP (5/11) The Pulse Pressure is a poor man's Swan-Ganz! As @FH_Verbrugge beautifully explained, looking at the PP and DBP together helps you understand the pathophysiology behind a patient with acute decompensated heart failure.
1
8
33
(3/11) @NephroP showed us how VEXUS parameters correlate with improvement in kidney function and electrolytes when decongestion is initiated. Do not be fooled into thinking that someone with “no pitting edema” does not require decongestion.
1
5
21
(1/11) A week after having the opportunity to co-organize #HR25, I had some time to reflect on my top 10 learning points. Please give it a read 👇.
3
27
59